5 Obstetric Ultrasound
5.1 Learning Objectives
After reviewing this chapter, you should be able to do the following:
- Understand the embryologic development in the first, second, and third trimesters.
- Examine various fetal structures and identify abnormalities.
5.2 Introduction
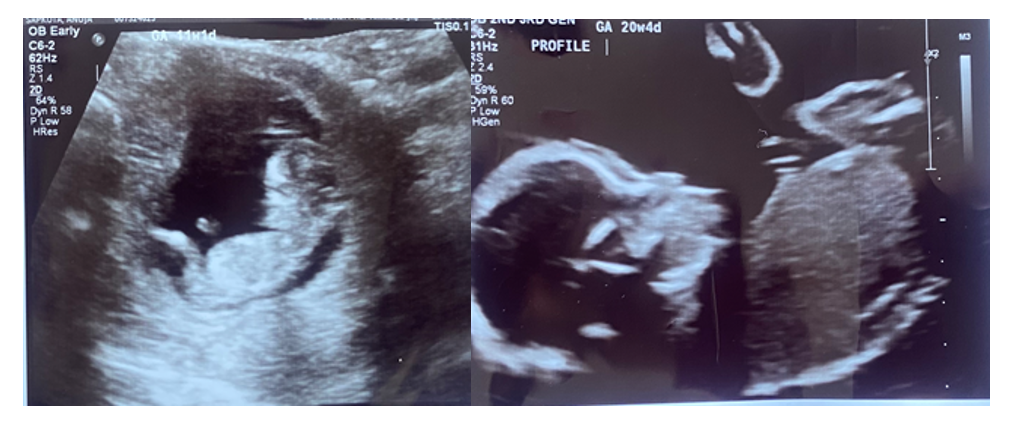
The exciting notion that an individual organism has embryologic development that reflects the species’ evolutionary development has been a theory that is present not only in science but also in other fields such as language and music. With the use of ultrasound, we will be able to observe the incredible development of a fertilized ovum into an infant. An example of this transition has been shown in Figure 5-1.
5.3 Role of Ultrasound in Obstetrics
Obstetrics encompasses some of the same considerations as adult diagnostic ultrasound with a critical addition: rapid growth. There is no other time in life when various organs’ functionality is time dependent. The developmental changes in early organ growth are part of the most fascinating differentiation process. What is being observed within a specific imaging procedure in utero, although completely normal, actually changes over time. Broken down further, findings at specific gestational times depend on the level of differentiation an organ has undergone at a specific time in gestational development.
The accuracy of ultrasound is variable, and the issue of diagnostic accuracy is essential to understand for any medical professional. Sensitivity and specificity are commonly used quantitative measures to report such accuracy. For a given test and disease/condition, sensitivity is the ability of the test to correctly identify something being positive. Its specificity for a given test and disease/condition is how well it can distinguish those with disease from those without.[1] Expressed as equations, the calculations may be done as follows:
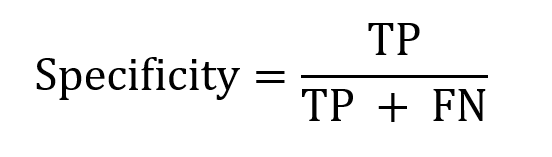
and
where
- true positive (TP) results when an imaging test is positive, and the patient has the disease/condition;
- false positive (FP) results when an imaging test is positive, and the patient does not have the disease/condition;
- true negative (TN) results when an imaging test is negative, and the patient does not have the disease/condition; and
- false negative (FN) results when an imaging test is negative, and the patient has the disease/condition.
In recent years more than ever, another consideration is the cost of medical interventions. Clinicians should have a good idea of the impact of the tests that they order:
-
- How much does a test cost the patient and society?
- What is the sensitivity and specificity of each test?
- Will the test results aid in the care of the patient?
An example of a standard test is the complete blood count (CBC). The CBC is relatively inexpensive, reproducible among different labs, and often clinically helpful. The sensitivity of the CBC is regarded as relatively high. The specificity is often not very high. On this latter point, an elevated CBC can often be one of the first and most important clues to an impending worsening of an infectious process such as appendicitis. An elevated CBC can also be considered a “false positive” caused by medicines such as steroids or endogenous epinephrine secretion (for example, if the patient recently experienced a traumatic event). In the early stages of pregnancy, a CBC test can help determine various health abnormalities, including anemia and infections.
Maternal-fetal medicine specialists and their specialized technicians understand fetal development and testing rationales to make truly unique diagnoses. It is not unusual for heart development to be assessed weekly or even more frequently when difficulties are suspected, as cardiac problems can develop as gestation progresses. The following basic assessments are commonly performed in obstetrics ultrasound.
5.3.1 Amniotic Fluid Assessment
The volume of amniotic fluid is calculated by what is called the amniotic fluid index. Even debris (represented by diffuse abnormal reflections in the amniotic fluid) is a harbinger of difficulties. At first glance, the ease of clarity and measurement is heavily influenced by the amount of amniotic fluid. As discussed in the earlier chapters, media, especially fluid, influences the quality of ultrasound wave transmission and reflection. Figure 5-2 shows an ultrasound image at 23 weeks of the fetus, amniotic fluid, and normal fetal morphology. A clear initial view is not necessarily a good sign, since excess amniotic fluid (a condition referred to as polyhydramnios) may make the images easy to obtain but may, more importantly, indicate problems. It has been noted that polyhydramnios represents a high-risk obstetric condition as much as 20% of the time.[2],[3]

5.3.2 Heart Rate and Heart Development
Fetal cardiac development (the development of the four chambers) is fascinating. The normal opening between the two upper chambers of the fetus’s heart, the right and left atria, is called the foramen ovale (FO). The FO permits blood flow to bypass the lungs before the infant is born (a fetus gets its oxygen from the placenta, not the lungs). As a result, the heart does not have to work as hard to pump blood where it is not needed. The FO typically closes six months to a year after the infant is born. A patent foramen ovale (PFO) occurs when the FO remains open after birth. A PFO often does not cause any issues.[4] When an infant is born with congenital heart abnormalities, the FO is more likely to remain open.
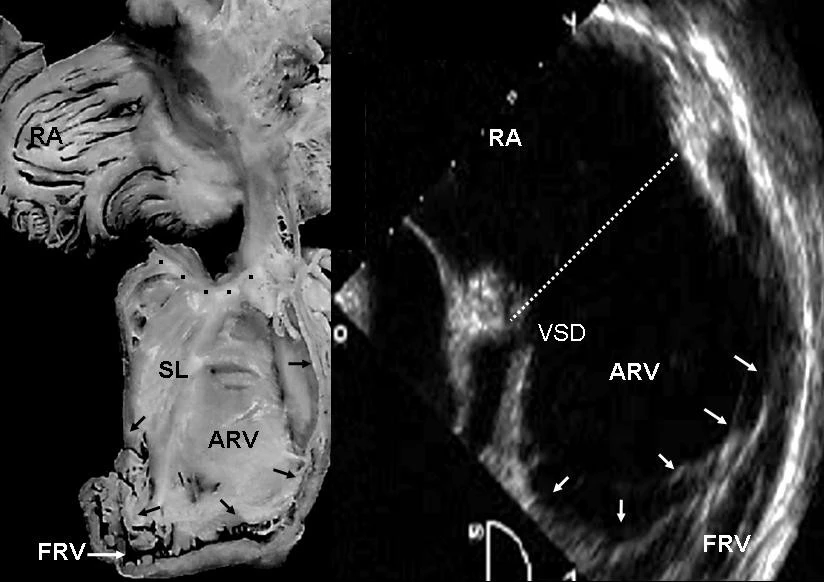
There is a division of a single atrium and a single ventricle by the growth of a septal wall from the wall of the single cavity in all directions toward the middle. This is a gradual and persistent hole in the septum that grows abnormally, leading to the septum closing, which results in a septal defect. Fortunately, one can detect both an atrial septal defect and/or a ventricular septal defect using ultrasound, as shown in Figure 5-3. Color flow ultrasound Doppler is often helpful, as one can view the flow from one side of the dividing atrial atrium or ventricle to the other side.
5.3.3 The Relationship Between the Maturity of Different Organs
Different gestational sizes of different organs in the same fetus can indicate genetic and fetal nutritional problems. Intrauterine Growth Retardation (IUGR) can be either symmetric or asymmetric:
(A) Symmetric indicates a genetic or chromosomal difficulty. The term symmetric refers to the abnormal influence (mostly delayed growth) that affects all organs equally. It is essential to correctly postulate why a symmetric IUGR is often more reversible. Ultrasound-guided intrauterine blood transfusion is often used to improve IUGR in earlier fetal life.
(B) Asymmetric indicates that the head/brain is of the expected size but the baby’s body size and other measures, such as the abdominal circumference, are relatively small. This often indicates poor growth due to inadequate umbilical cord perfusion or anemia.
5.3.4 Skeletal Growth Development
Spinal vertebra development, or lack thereof, can be the first diagnostic clue to spina bifida. Without normal closure, the thecal sac enveloping the spinal cord in the vertebra may be seen to be bulging outside of the vertebrae. Limb development can be noted to have an abnormally small size or an abnormal shape.
5.3.5 Genital Development
Genital development, more than ever before, may be evaluated before delivery. This is made possible by the higher resolution of high-end obstetric ultrasound machines.
5.3.6 Fetal Activity
The fetus’s activity can indicate variable states ranging from fetal distress to the infant sleeping. The biophysical profile (BPP) calculates different aspects of fetal motion that indicate fetal well-being. If the fetus has an abnormally low BPP, and especially if the fetus is mature enough to do well outside of the uterus, delivery is often induced or a cesarean is performed.
5.4 Prenatal Ultrasound
Prenatal ultrasound has a continuing rapid pace of development with the advent of 3D and 4D technology. The debate regarding both the usefulness of prenatal ultrasound in terms of the wise expenditure of health care dollars and diagnostic accuracy has lagged behind the explosion of technology. We are charmed by babies, and rightfully so. The development of prenatal ultrasound will no doubt continue and will hopefully benefit humanity.
The subject of prenatal ultrasound allows some discussion about the considerations of technological development. With the development of the prenatal ultrasound technique come widespread expectations and assumptions that may not be true. First, with the demonstrable development of a new technology, it is assumed to work for the intended purpose. It is easy for a layperson to believe that such sophisticated modalities would be 100% accurate and, therefore, worth it. For prenatal ultrasound, it would be predicted that a clear picture would allow for not only accurate prenatal diagnosis but meaningful intrauterine treatment of most conditions. The truth of this assumption is variable, depending, of course, on the condition being evaluated. The greatest accuracy of diagnosis has to do with conditions related to abnormality of amniotic fluid volume. The most discouraging levels of accuracy have to do with the detection of heart defects and isolated congenital abnormalities such as a cleft palate. This subject quickly becomes more complex as one progresses into discussions about issues such as the sensitivity index, cumulative Gaussian distribution, and dimensionless statistics.
5.4.1 Evaluation of Abnormalities
If abnormalities are accurately discovered, the next hurdle is finding an effective treatment. Routinely in sophisticated medical centers, maternal-fetal medicine specialists and perinatologists perform procedures such as amniotic blood transfusions, fetal ureteral valve repair, and removal/replenishment of amniotic fluid volume due to abnormalities. In individual cases, there have been unbelievable advances and actual lives saved with this sophisticated technology. In our ever-cost-sensitive environment, we must balance this incredible cost against the expenditures of limited dollars for patient education.
5.4.2 Evaluation of Embryological Development
The first trimester of pregnancy is when there is the most danger of mishap. Due to the rapid cell division and differentiation of the embryo in unbelievable numbers, even minor “errors” in cellular division may cause the very common event of spontaneous abortion. In the emergency department, it is often an unhappy task for a health professional to explain this issue to patients and their families. It is essential to be careful in doing so due to the tendency of many patients to wonder why a tragedy has occurred and to cast blame on themselves. Without careful explanation, patients who experience spontaneous abortion, or expulsion of an unsuccessful pregnancy through the vagina, may feel that they were at fault when this is not the case.
One can evaluate the earliest pregnancies with many parameters. The serial evaluation of the lab value of the “pregnancy hormone,” beta human chorionic gonadotropin (BHCG), over a few days gives an indication of developmental health. Early in pregnancy, the BHCG should double every 2–3 days. If there is a decrease or no increase in the value, this is a most worrisome sign for embryologic death. Often, early fetal demise will not be 100% certain, and the ultrasound and BHCG evaluation are done serially over a few days. Two ultrasounds without a heartbeat at the appropriate fetal age and an inappropriately declining BHCG are often considered diagnostic for intrauterine fetal death and likely spontaneous abortion.
Ultrasound evaluation can most accurately begin in early pregnancy with a longer, higher-frequency transvaginal probe. Returning to the knowledge of ultrasound physics from earlier chapters, it is crucial to realize why a higher-frequency probe is placed through the vagina and near the cervix. The accuracy of the higher-frequency probe allows a marked improvement in resolution when the reflection is only a short distance. At four to five weeks gestation, we first see the fetal yolk sac, fetal pole, gestational sac, and fetal heartbeat. An irregularly shaped gestational sac or lack of a fetal heartbeat when the embryologic or crown-rump length is greater than five weeks are ominous signs of possible embryological death. It is estimated that up to 50% of pregnancies end in spontaneous abortion, often so early in development that the patient does not recognize the pregnancy.

The other common peril in the first trimester of pregnancy is ectopic pregnancy, or pregnancy outside the uterus. As with intrauterine pregnancies, ectopic pregnancies grow and develop at very fast rates. Figure 5-4 shows an ectopic pregnancy adjacent to the left ovary. Most ectopic pregnancies are in the ovaries, fallopian tubes, or uterine horn. In either event, the pregnancies can “outgrow their blood supply,” rupturing and leading to maternal hemorrhage and potential death.
Sonographic signs of an intact ectopic pregnancy include enlargement in the area of implantation (even a functioning fetal heartbeat) and an “empty uterus” or lack of an intrauterine pregnancy when the BHCG is greater than 1500 international units. A patient with a ruptured ectopic pregnancy classically presents with sudden-onset unilateral pelvic pain and possibly signs of hemorrhagic shock. On the ultrasound, free fluid may be noted most commonly not only in the pouch of Douglas but also in the paracolic gutters or Morrison’s pouch. This is often a surgical emergency; the bleeding must be stopped before maternal death occurs from hemorrhage.
Gestational dating refers to the estimation of the gestation of the pregnancy. This is somewhat helpful when the medical provider evaluates issues such as whether to try to delay a patient in preterm labor or if induction of a patient who continues pregnancy more than 10 days after the estimated date of confinement (EDC) is indicated. Both of these issues have several determining factors. For preterm labor, infant mortality significantly decreases as delivery is delayed in many cases. For postterm situations, having a healthy term fetus more than 10 days after the EDC may pose unnecessary risks. These are complex decisions based on such data. To further complicate the issue, gestational dating may have variable accuracies. Some individuals have little or no prenatal care (i.e., some show up only to the emergency department when they are about to deliver or deliver at home without ever being evaluated by a medical provider). If one does have prenatal care and prenatal ultrasound, gestational dating accuracy remains variable. The facet that introduces the most variability is the gestational age at which the scan is performed. It has been traditionally noted that gestational dating accuracy has an 8% variability of the maturity of the pregnancy.[5] An example is that a 45-day gestation would have an accuracy of ±3.5 days, and a pregnancy of approximately 250 days would have an accuracy of ±20 days. This variability may decrease as ultrasound machines become more sophisticated. The principle, however, continues to make sense that as pregnancies mature, the genetic and environmental issues that make us all different have a greater influence on growth.
5.5 The Second and Third Trimester
At approximately 14 weeks gestation, evaluation of organogenesis becomes more useful. As there is fetal growth, there is predictably more accuracy but fewer chances for potential interventions that may help as pathologic damage becomes irreversible. Organogenesis evaluation may differ according to the medical circumstances. Diagnostic capabilities vary according to the operator and machine.
The head, heart chambers, lungs, abdominal organs, genitals, and bones may be more successfully evaluated in the second trimester. While diagnostic accuracy improves, individual organs remain the most difficult to evaluate. Detecting some prenatal heart defects is an area of great interest and some improvement. The most common advantage of prenatal diagnosis of congenital heart defects is that if the condition is known, in more developed countries, the delivery can often be done at a tertiary medical center where there are maternal-fetal medicine specialists, pediatric cardiologists, pediatric surgeons, neonatal ventilators, and other sophisticated options for immediate treatment.
Warda et al.[6] are originally credited with developing regression analysis values to use fetal growth parameters to estimate gestational age. Due to an interesting phenomenon known as “organ sparing,” some organs are more reflective of accurate gestational dating than others. If there is placental insufficiency, the head will continue to grow more normally, but abdominal growth will lag. This increasing discrepancy between fetal head and abdominal growth may lead to the diagnosis of IUGR and indicate induced delivery of a small or preterm infant.
5.5.1 Head Evaluation
The head measurement is first determined by the biparietal diameter and occipital-frontal circumference. There is a flow pattern of cerebrospinal fluid (CSF) through the brain’s ventricular system and into the spinal cord through the foramen of Magendie and the foramen of Luschka. An obstruction of this flow causes increased back pressure, dilation of the ventricles, and pathologic pressure of the surrounding brain tissue. Many other conditions other than stenosis of the foramina cause hydrocephalus. This abnormality may be seen on prenatal ultrasound first as an increased head size and then as an increased ventricular size. Figure 5-5 shows an ultrasound image of fetal hydrocephalus. Hydrocephalus intervention is most often treated with postdelivery shunt placement, which involves placing a tube in the cerebral ventricles to bypass the obstruction and drain the excess fluid into other body cavities, such as the abdomen, where the fluid may be reabsorbed.

Other than abnormalities in CSF flow, there may be other abnormalities that are represented by an abnormal prenatal head ultrasound. These abnormalities have a wide range of etiologies, including genetic abnormalities, congenital abnormalities, and abnormal growth in an otherwise normal fetus. Genetic abnormalities have to do with abnormal chromosomes primarily due to mutation. Congenital abnormalities usually begin in the prenatal period and are evident at birth.
Cardiac ultrasound accurately predicts congenital abnormalities for many more subtle conditions. The most common congenital heart disease is patent ductus arteriosus, where the fetal ductus arteriosus that diverts the circulation away from the prenatal lungs and into the aorta does not close upon birth. This, of course, is never diagnosed prenatally. Rare but hazardous and sometimes fatal conditions such as transposition of the great vessels or defects of the central cardiac wall (called the septal wall) may be undetected by screening ultrasound exams. The complexity increases when there are combinations of heart defects such as tetralogy of Fallot, including pulmonary stenosis, right ventricular hypertrophy, ventricular septal defect, and an aorta that receives blood from both the right and left ventricle. In developed countries, when a fetal cardiac ultrasound is suspected from a routine prenatal ultrasound, a targeted ultrasound using more specialized machines and more specialized operators is subsequently performed. There may also be noncardiac prenatal ultrasound signs of heart disease, such as fetal hydrops (swelling) for fetal congestive heart failure.
5.5.2 Abdominal Exam
Most intrauterine conditions that are treatable prior to delivery are identified in the abdominal exam. The umbilical cord is utilized as a site of intrauterine blood transfusions (by maternal-fetal specialists) to correct fetal anemia and hypovolemia. This procedure is done under real-time ultrasound and may be genuinely lifesaving as well as preventative of anomalies such as Potter’s sequence.
The fascinating development of the normal kidneys involves the division and migration of one central organ into a right and left kidney. Abnormalities in this separation and division include the persistence of the larger central organ, called a “horseshoe kidney.” Difficulties in renal function, such as nonfunction, may be suspected when the kidney appears small or atrophic. If a kidney is obstructed but functioning, “backward pressure” from the fetal urine may cause the kidney to enlarge, a condition known as hydronephrosis.
Some urinary tract obstructions may be corrected by intrauterine surgery. Posterior urethral valves in the male are the most common correction. When successful, relieving the obstruction prevents further renal damage and restores the average amniotic fluid volume to prevent complications from abnormal pressure.
5.5.3 Amniotic Fluid
Evidence of the normal flow of amniotic fluid is indicated by amniotic fluid volume. Contributions to the average amniotic fluid volume are mostly from fetal urine production, with some contributions from umbilical cord filtrate. Detraction from the amniotic fluid volume is mainly from fetal swallowing and fetal aspiration of the amniotic fluid into the lungs.
Oligohydramnios, a condition caused by reduced amniotic fluid volume from the reduced contribution of urine, creates well-known fetal anomalies called Potter’s sequence. This condition is described as including particular fetal facial characteristics, fetal limb abnormalities, and pulmonary hypoplasia. The limb abnormalities are from abnormal pressure.
Polyhydramnios may be from inadequate fetal swallowing of amniotic fluid, inadequate fetal aspiration of amniotic fluid, or fetal gastrointestinal obstruction that prevents amniotic fluid from progressing once swallowed.
5.5.4 Femur Bone Length
The femur length is often considered to be the most reliable indicator of gestational age. Congenital abnormalities of the femur that make this statement not 100% true are rare and often apparent, as the femur abnormality coexists with other skeletal difficulties.
5.6 Tertiary Ultrasound Exams
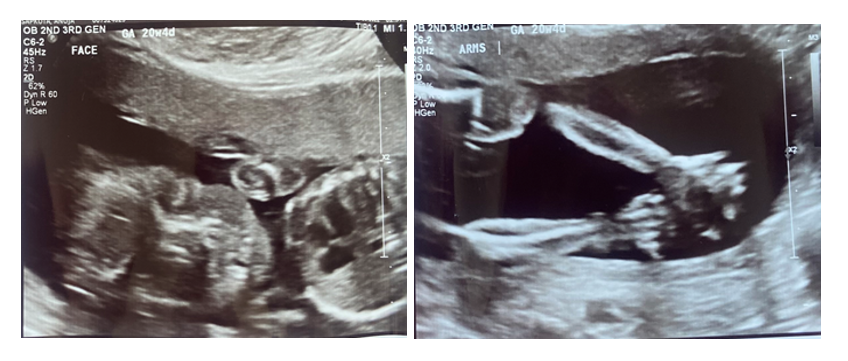
In first discussing the more common screening prenatal ultrasound exams, we have made mention of more targeted exams. Thoracic measurements, measurement of bones other than the femur, more targeted cardiac exams, more central nervous system ventricular evaluations, and fetal neck skin thickness measurements are made. For example, Figure 5-6 shows ultrasound images of a fetus’s face and arms during week 20.
More specific investigation of suspected abnormalities may indicate some conditions that can be corrected prenatally by thrilling advanced treatments such as umbilical cord blood transfusions, correction of amniotic fluid abnormalities, relief of posterior ureteral valve abnormality, or other intrauterine surgeries. As discussed earlier, almost all of these procedures are initiated by the targeted ultrasound.
In 2023, as in every other year in the history of humanity, it remains true that the results of the most sophisticated events in fetal development can be influenced by some of the simplest yet sometimes neglected measures: receiving good prenatal care, ceasing maternal smoking or other substance use, and taking prenatal vitamins. We believe that it is important for future clinicians reading this to never tire of reminding patients to optimize their developing infants’ likelihood of being healthy.
5.7 Self-Assessment
- Define sensitivity and specificity in the context of prenatal ultrasound.
- In early pregnancy, how often should the beta human chorionic gonadotropin (BHCG) double, typically?
- What are three forms of abnormalities that can be identified by performing a prenatal head ultrasound?
- What measurements does the tertiary ultrasound exam include?
5.8 Further Readings
- Acton CM. The use of ultrasound in pregnancy. Aust Fam Physician. 1997 Mar;26(3):239–43. PMID: 9078656.
- Whitworth M, Bricker L, Mullan C. Ultrasound for fetal assessment in early pregnancy. Cochrane Database Syst Rev. 2015 Jul 14;2015(7):CD007058. doi: 10.1002/14651858.CD007058.pub3. PMID: 26171896; PMCID: PMC6464767.
- AIUM-ACR-ACOG-SMFM-SRU Practice Parameter for the Performance of Standard Diagnostic Obstetric Ultrasound Examinations. J Ultrasound Med. 2018 Nov;37(11):E13–E24. doi: 10.1002/jum.14831. Epub 2018 Oct 11. PMID: 30308091.
- Salomon LJ, Alfirevic Z, Bilardo CM, Chalouhi GE, Ghi T, Kagan KO, Lau TK, Papageorghiou AT, Raine-Fenning NJ, Stirnemann J, Suresh S, Tabor A, Timor-Tritsch IE, Toi A, Yeo G. ISUOG practice guidelines: Performance of first-trimester fetal ultrasound scan. Ultrasound Obstet Gynecol. 2013 Jan;41(1):102–13. doi: 10.1002/uog.12342. Erratum in: Ultrasound Obstet Gynecol. 2013 Feb;41(2):240. PMID: 23280739.
- Morgan M, Sciacca F, Knipe H. Sensitivity and specificity. Radiopaedia [internet]. [date unknown] [cited 2023 Oct 28]. Available from: https://doi.org/10.53347/rID-34845. ↵
- Hwang DS, Mahdy H. Polyhydramnios. [Updated 2023 Feb 20]. In: StatPearls [internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562140/ ↵
- Hamza A, Herr D, Solomayer EF, Meyberg-Solomayer G. Polyhydramnios: Causes, Diagnosis and Therapy. Geburtshilfe Frauenheilkd. 2013 Dec;73(12):1241–1246. doi: 10.1055/s-0033-1360163. PMID: 24771905; PMCID: PMC3964358. ↵
- Hampton T, Alsaleem M, Murphy-Lavoie HM. Patent Foramen Ovale. [Updated 2022 Sep 12]. In: StatPearls [internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493151/ ↵
- Committee Opinion No 700: Methods for Estimating the Due Date. Obstet Gynecol. 2017 May;129(5):e150-e154. doi: 10.1097/AOG.0000000000002046. PMID: 28426621. ↵
- Warda AH, Deter RL, Rossavik IK, Carpenter RJ, Hadlock FP. Fetal femur length: A critical reevaluation of the relationship to menstrual age. Obstet Gynecol. 1985 Jul;66(1):69–75. PMID: 3892390. ↵

