11 Focused Assessment With Sonography in Trauma (FAST) Exam
11.1 Learning Objectives
After reviewing this chapter, you should be able to do the following:
- Understand the importance of the FAST exam and the areas within the body that are assessed.
- Explore the various techniques used in the FAST exam.
11.2 Introduction
According to the National Trauma Institute, trauma accounts for 41 million emergency department visits annually and 2.3 million hospital admissions in the United States. The Focused Assessment with Sonography in Trauma (FAST) exam is a noninvasive, quick, and accurate evaluation using bedside ultrasound to identify free fluid, usually anechoic, such as blood in the pericardial, pleural, and peritoneal spaces.[1],[2] Specific indications include penetrating and blunt trauma to the chest, abdominal, and pelvic cavities. The low-frequency transducer is the most appropriate probe for the FAST exam. The patient is in a supine position. This is a simplified summary of a typical FAST examination assuming no trauma. It is imperative to first be familiar with a routine examination before examining for pathology.
11.3 Sonography for Trauma
As early as the 1990s, there was discussion in the literature regarding the usefulness of ultrasound in the rapid assessment of blunt trauma.[3] The natural advantage of ultrasound over pure clinical intervention is the accuracy of visualization, sensitivity (49–99% versus 27–45%), and specificity (95–100%). The advantage of ultrasound over CT scanning is the rapidity of the exam and the fact that the physician may remain at the bedside to make critical decisions regarding the potential rapidly changing condition of the patient. In a patient who has received blunt trauma (often from a motor vehicle accident) or penetrating trauma (such as a gunshot wound), the presence of free blood or free air in the abdomen may be seen within a few minutes by an experienced clinician.[4]
The original basis of trauma ultrasound was that the blood that escaped the vascular system due to trauma (e.g., bleeding inside the abdomen) would be seen as an abnormal hypoechoic entity in the abdomen. This concept is greatly aided by the fact that there are anatomic “potential spaces” where fluid, mostly extravascular blood, collects. Potential spaces had been known for centuries as locations where abnormal fluid collections could be reliably found and removed. It is with the more sophisticated radiology modalities that the fluid can be located before surgery and used diagnostically to help determine if surgery is necessary. Ultrasound imaging quickly and reliably indicates emergent surgery to stop the bleeding from a liver laceration, a splenic laceration, an ectopic pregnancy rupture, a bladder rupture, an injury to a major blood vessel, or less frequent injuries to other organs.
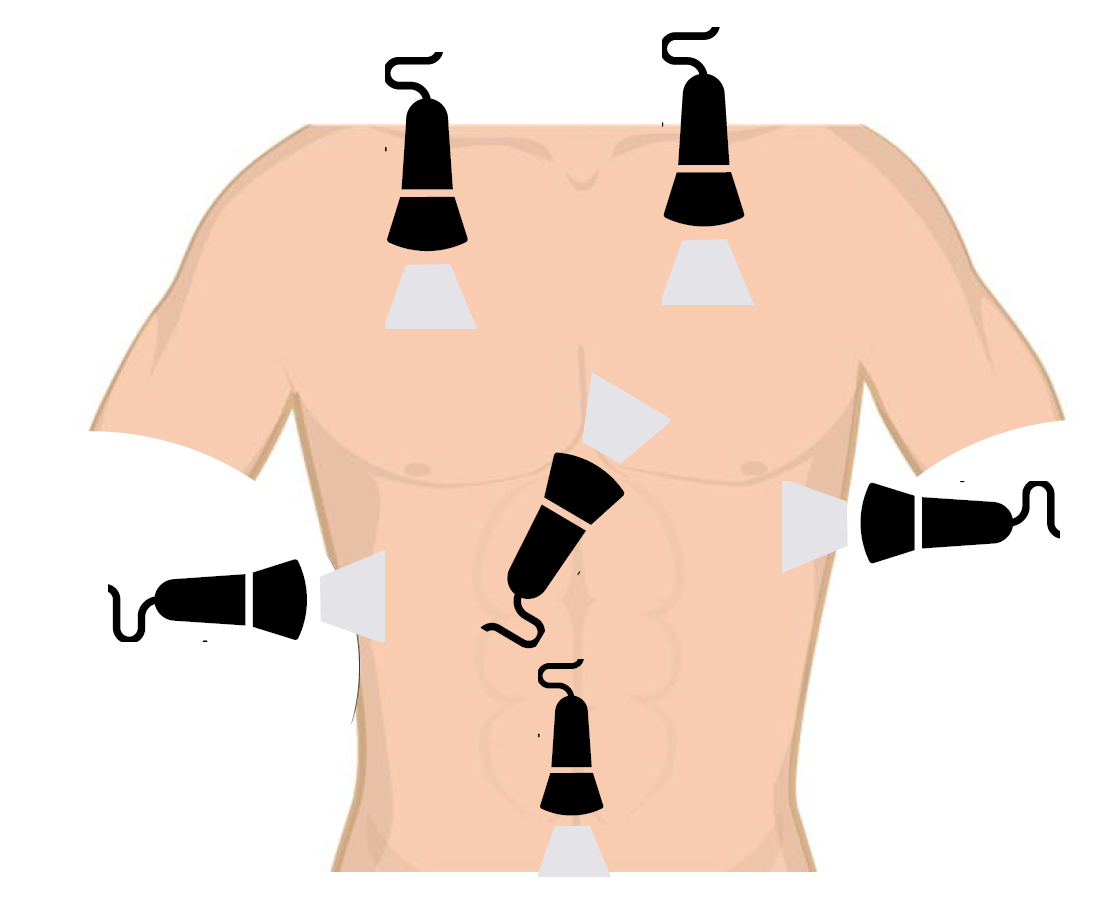
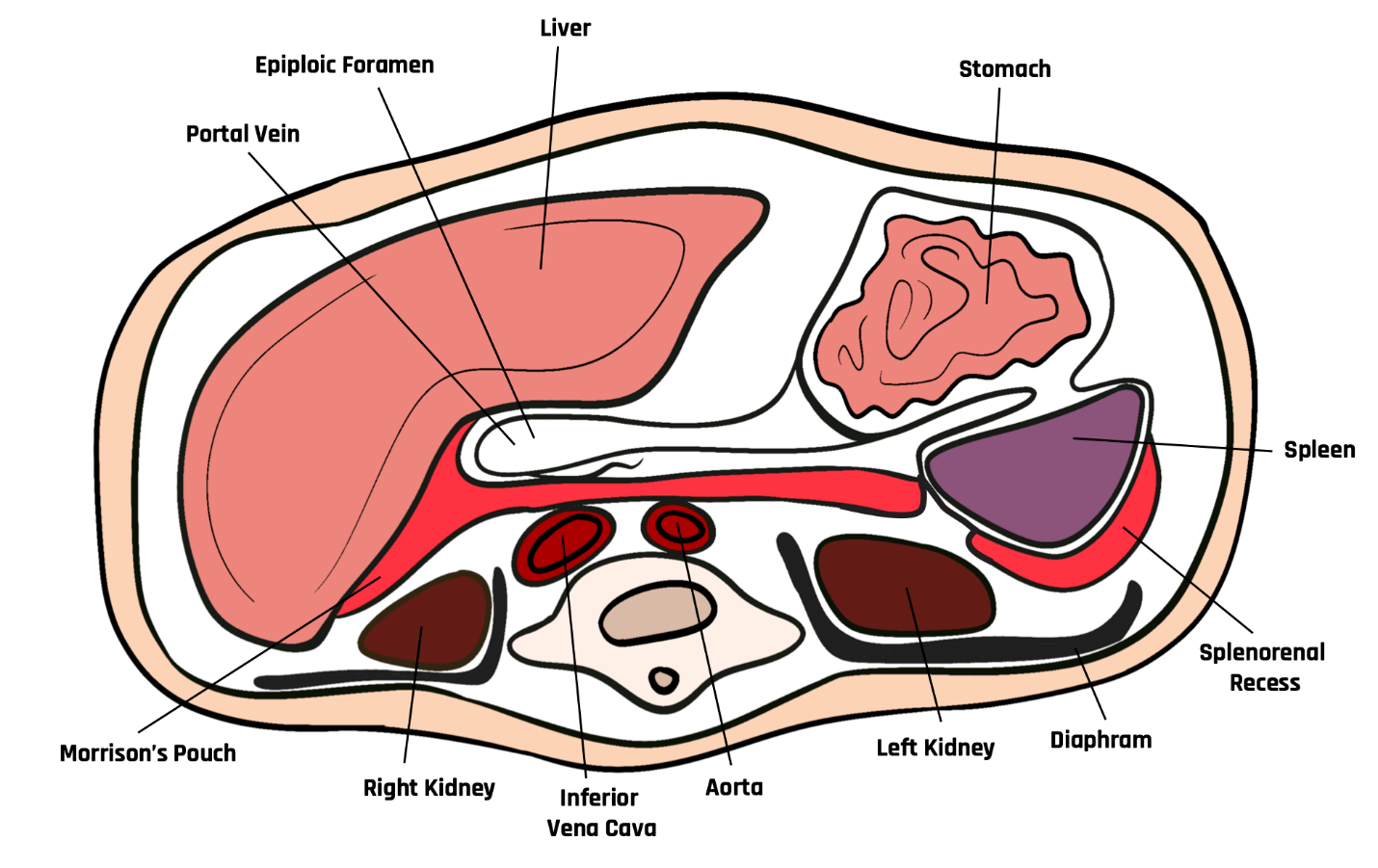
The FAST exam evaluates the right upper quadrant, the left upper quadrant, and the pelvis, as shown in Figure 11-1.[5] Most famous because of the more defined areas are Morrison’s pouch (in the right upper quadrant, highlighted by the contrasting bright, hyperechoic Gerota’s fascia) and the pouch of Douglas (in the low midline of the pelvis between the hyperechoic borders of the bladder in males or vagina in females superiorly and the rectum inferiorly). The splenic-renal recess in the left upper quadrants and the paracolic gutters in both the right and left lower quadrants are important to access but less easy to navigate.
The rapid ultrasound exam for trauma has extended to areas above the diaphragm as ultrasound has progressed. The eFAST (the extended FAST exam) also evaluates the lungs and heart[6] in addition to the abdomen, as shown in Figure 11-1. The probe is pointed superiorly from the xiphoid area to gain views of the heart and lungs. Again, the hypoechoic reflection of free, abnormal fluid is used as an indication of emergent surgery.
11.4 Techniques for the FAST Exam
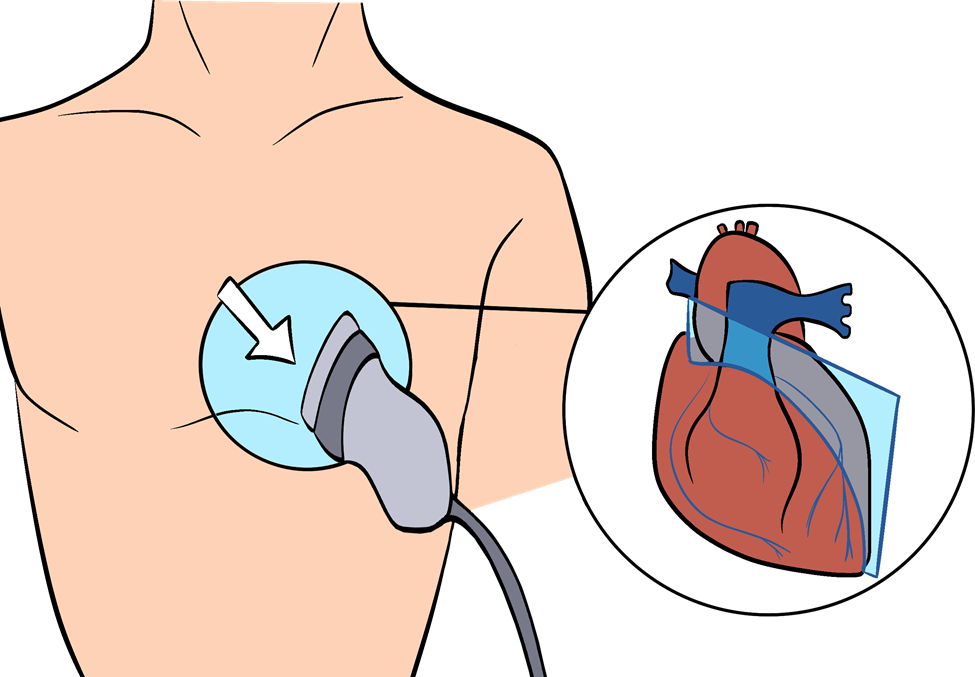
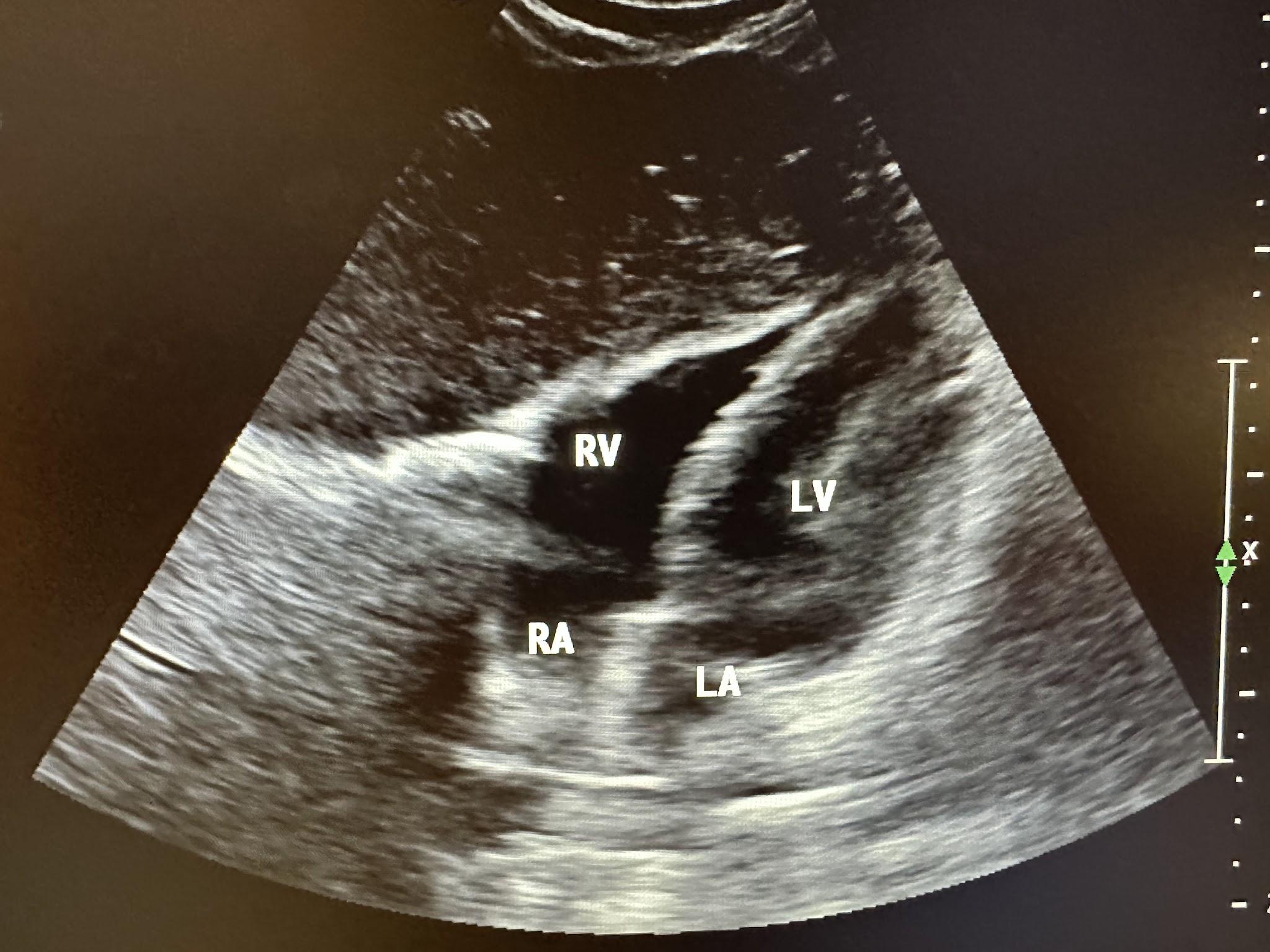
Above the diaphragm, this fluid collection indicates emergent action in the form of a pericardial or pleural effusion. In the case of pericardial effusion, cardiac tamponade can occur and must be treated immediately. Cardiac tamponade is a medical condition that causes the restriction of ventricular filling due to pressure of fluid in the pericardium. In the case of pleural effusion, the restriction is not the initial problem. However, there may be ongoing bleeding contributing to the effusion that must be stopped. Cardiac imaging is used to evaluate pericardial effusion. There are two different cardiac views. The parasternal long-axis view is obtained by placing the transducer just left of the sternum in the fourth or fifth intercostal space oriented to the right shoulder, as shown in Figure 11-2. The parasternal sagittal ultrasound view of the heart is shown in Figure 11-3. The abbreviations LV, RV, LA, RA, and A have been used for the left ventricle, right ventricle, left atrium, right ventricle, and aorta, respectively, in some of the following ultrasound images.
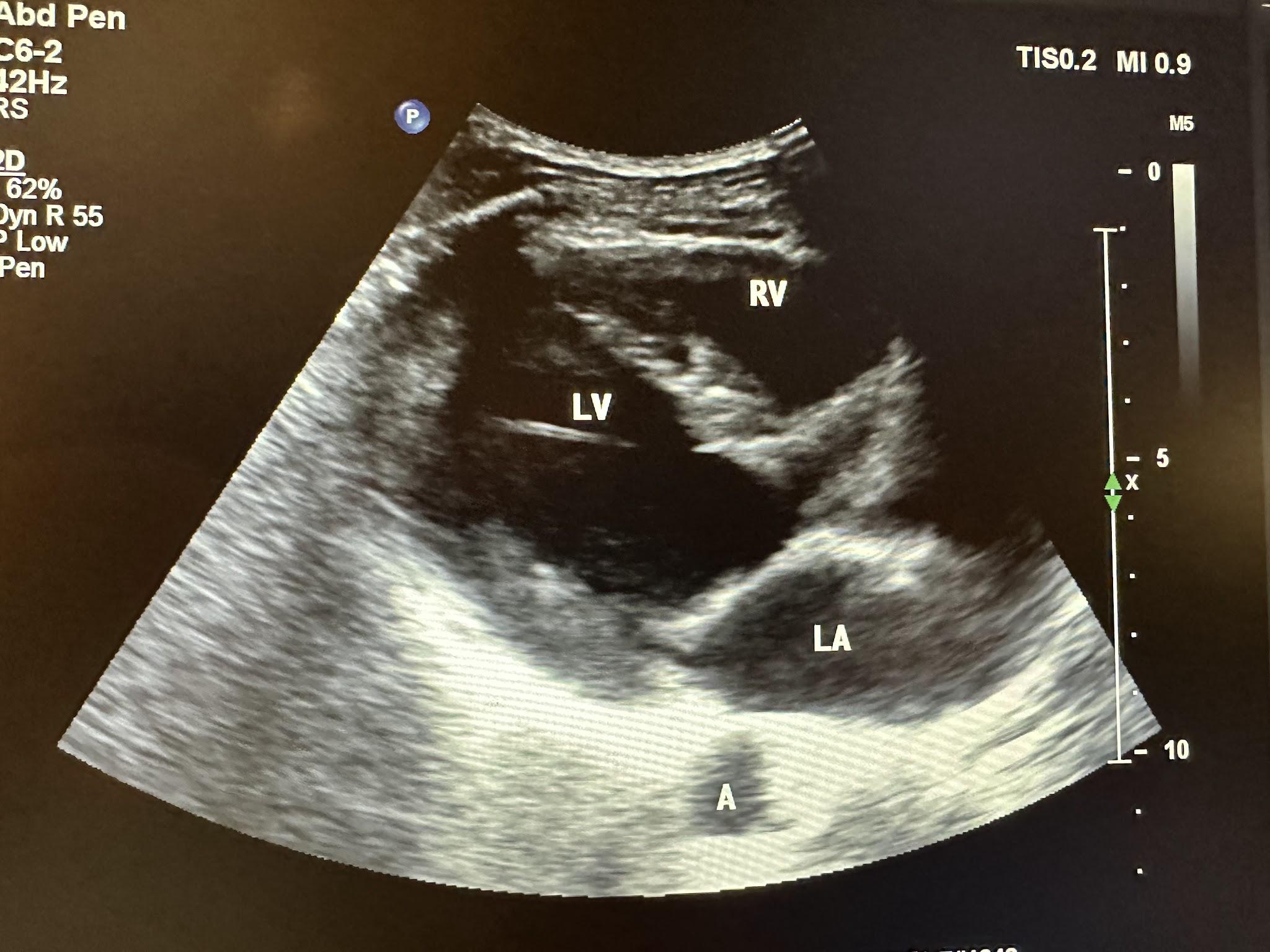
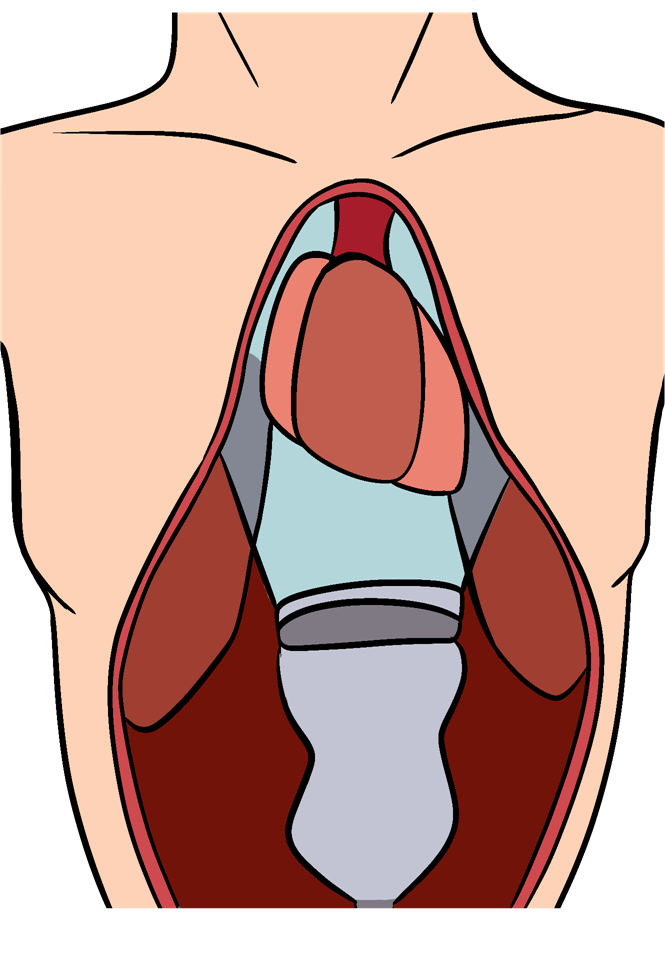
The subxiphoid view can sometimes be challenging in a patient who is considered obese. First, locate the xiphoid process, place the transducer down in a transverse position with the indicator facing toward the right, and aim between the head and left shoulder, as shown in Figure 11-4. Gently apply pressure downward, and visualize the cardiac contractility during respiration to identify the best visualization. Figure 11-5 shows the four-chamber view of the heart during this evaluation. Assess for hemopericardium, or fluid around the heart.
Pulmonary imaging in trauma has evolved over the years. Most recently, with the COVID-19 pandemic, it has become a more detailed and important part of the evaluation addressed in Chapter 8.
Peritoneal imaging of the abdomen/pelvis evaluates fluid in the hepatorenal recess (also referred to as Morrison’s pouch), splenorenal recess, and pelvic cavity. Figure 11-6 shows a cross-sectional diagram of the abdomen, demonstrating Morrison’s pouch (hepatorenal recess) and the splenorenal recess. The most straightforward abdominal view is to place the transducer in the midaxillary line at the 8th to 11th intercostal space with cephalad orientation.
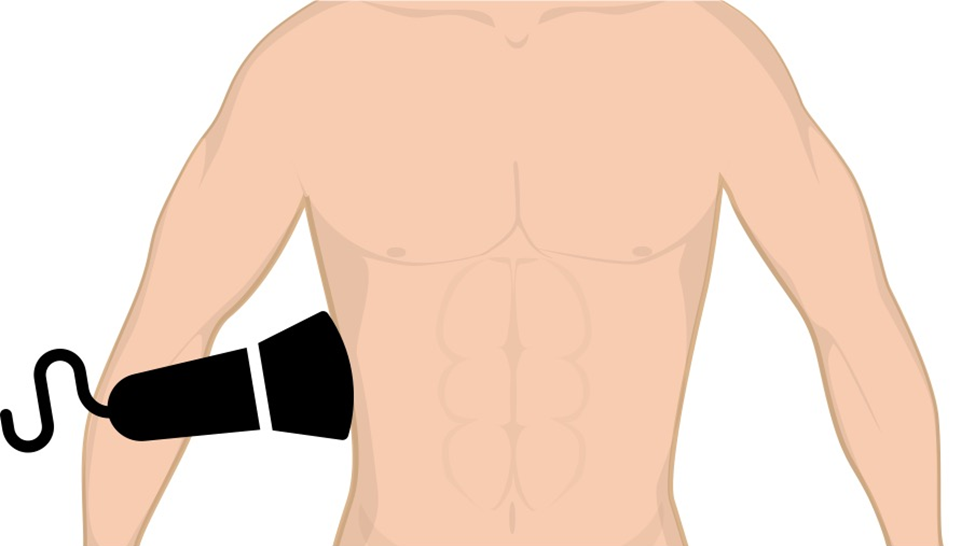
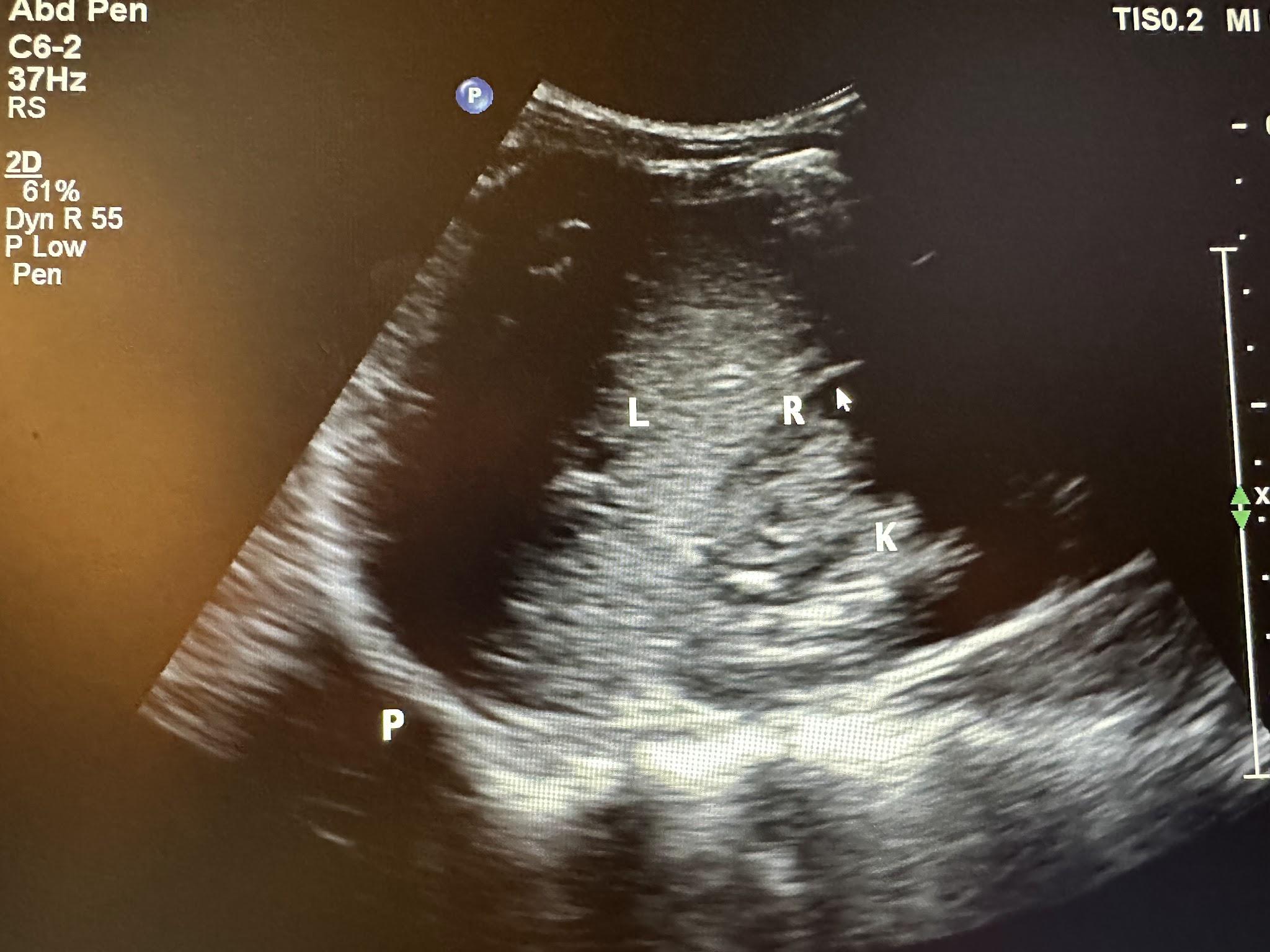
First, start on the right abdominal region in the midaxillary line between the 8th to 11th intercostal spaces, as shown in Figure 11-7. Maneuver the transducer by sliding, fanning, angling, and rotating until you can visualize the liver and kidney well. The abbreviations L, R, K, P, and S have been labeled in some of the following ultrasound images, representing liver, recess (hepatorenal and splenorenal), kidney, pleura, and spleen, respectively. Figure 11-8 represents the hepatorenal view, showing the liver, hepatorenal recess, kidney, and pleura.
Next, place the transducer in the longitudinal plane with the indicator facing the patient’s head, evaluating between the fifth to ninth intercostal spaces, as shown in Figure 11-9. Again, maneuver the transducer until you can visualize the spleen and kidney well. Figure 11-10 represents the splenorenal view, showing the spleen, splenorenal recess, and kidney.

The pelvic cavity also has an area where peritoneal fluid can collect within the pouch. In women, it is called the rectouterine pouch or pouch of Douglas (peritoneum between the rectum and uterus). In men, it is referred to as the rectovesical pouch (peritoneum between the rectum and bladder), as shown in Figure 11-11.
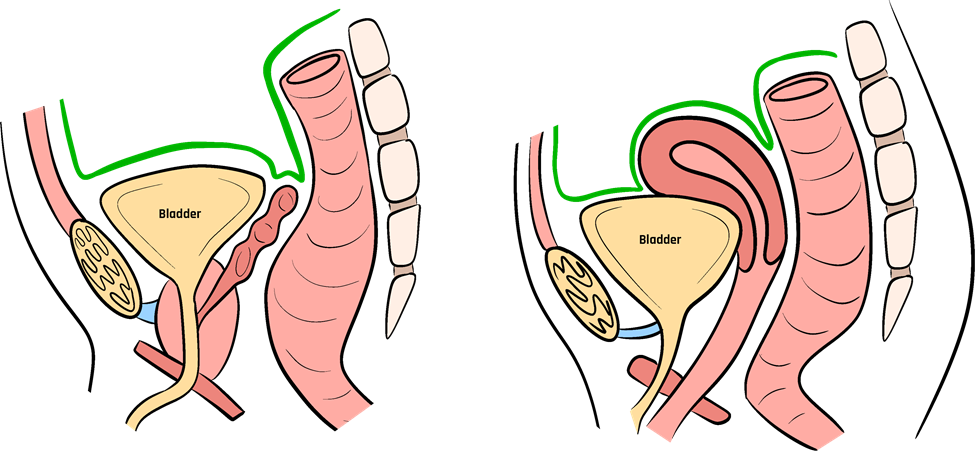
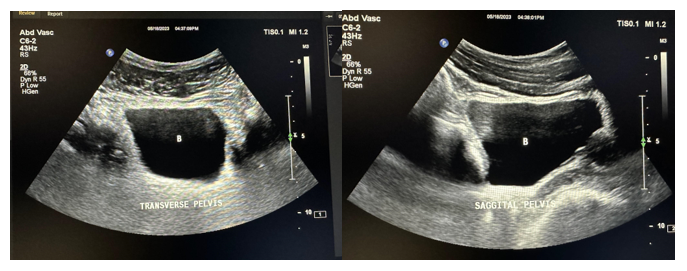
Figure 11-12 shows an ultrasound image of the bladder (abbreviated B on the image) obtained by placing the transducer in the patient’s midline, right above the pubic symphysis. This concludes the eFAST exam.
The best time to stop bleeding is as soon as possible. When the bleeding is not apparent or external, ultrasound has made leaps of progress regarding rapid diagnosis. The first hour after trauma, known as the “Golden Hour of Trauma,” is a recognized time entity in which medical professionals aim to provide definitive care. In the future, it may well be a standard of care for paramedics to perform ultrasound on the scene. In this case, the image will be transmitted to an emergency department and a trauma surgeon’s cell phone so that preparations for emergent surgery may be made before the patient arrives. Perhaps in the future, the patient will be taken immediately off the ambulance and directly to surgery. Trials of this technology are ongoing all over the world.
11.5 Self-Assessment
- What is the original basis of the FAST or eFAST ultrasound exam for trauma?
- At what position does one place the transducer for the parasternal long-axis cardiac view in the FAST exam?
- How does one proceed to see the subxiphoid view in a patient who is obese, which is sometimes challenging to obtain?
- What anatomical structures do the peritoneal imaging in the FAST exam evaluate?
- What is another name for the hepatorenal recess?
11.6 Further Readings
- Haskins SC, Bronshteyn Y, Perlas A, El-Boghdadly K, Zimmerman J, Silva M, Boretsky K, Chan V, Kruisselbrink R, Byrne M, Hernandez N, Boublik J, Manson WC, Hogg R, Wilkinson JN, Kalagara H, Nejim J, Ramsingh D, Shankar H, Nader A, Souza D, Narouze S. American Society of Regional Anesthesia and Pain Medicine expert panel recommendations on point-of-care ultrasound education and training for regional anesthesiologists and pain physicians-part II: Recommendations. Reg Anesth Pain Med. 2021 Dec;46(12):1048–1060. doi: 10.1136/rapm-2021-102561. Epub 2021 Feb 24. PMID: 33632777.
- Noble VN, Nelson BP. Manual of Emergency and Critical Care Ultrasound. 2nd ed. New York: Cambridge University Press; 2011. p. 360.
- Williams SR, Perera P, Gharahbaghian L. The FAST and E-FAST in 2013: Trauma ultrasonography: Overview, practical techniques, controversies, and new frontiers. Crit Care Clin. 2014 Jan;30(1):119–50, vi. doi: 10.1016/j.ccc.2013.08.005. PMID: 24295843.
- Griffin XL, Pullinger R. Are diagnostic peritoneal lavage or focused abdominal sonography for trauma safe screening investigations for hemodynamically stable patients after blunt abdominal trauma? A review of the literature. J Trauma. 2007 Mar;62(3):779–84.
- Desai N, Harris T. Extended focused assessment with sonography in trauma. BJA Educ. 2018 Feb;18(2):57–62. doi: 10.1016/j.bjae.2017.
- Bloom BA, Gibbons RC. Focused Assessment With Sonography for Trauma. [Updated 2023 Jul 24]. In: StatPearls [internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470479/ ↵
- Williams SR, Perera P, Gharahbaghian L. The FAST and E-FAST in 2013: Trauma ultrasonography: Overview, practical techniques, controversies, and new frontiers. Crit Care Clin. 2014 Jan;30(1):119–50, vi. doi: 10.1016/j.ccc.2013.08.005. PMID: 24295843. ↵
- Pearl WS, Todd KH. Ultrasonography for the initial evaluation of blunt abdominal trauma: A review of prospective trials. Ann Emerg Med. 1996 Mar;27(3):353–61. doi: 10.1016/s0196-0644(96)70273-1. PMID: 8599497. ↵
- Boulanger BR, McLellan BA, Brenneman FD, Wherrett L, Rizoli SB, Culhane J, Hamilton P. Emergent abdominal sonography as a screening test in a new diagnostic algorithm for blunt trauma. J Trauma. 1996 Jun;40(6):867–74. doi: 10.1097/00005373-199606000-00003. PMID: 8656471. ↵
- Rozycki GS, Shackford SR. Ultrasound, what every trauma surgeon should know. J Trauma. 1996 Jan;40(1):1–4. doi: 10.1097/00005373-199601000-00001. PMID: 8576968. ↵
- Kirkpatrick AW, Sirois M, Laupland KB, Liu D, Rowan K, Ball CG, Hameed SM, Brown R, Simons R, Dulchavsky SA, Hamilton DR, Nicolaou S. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: The Extended Focused Assessment with Sonography for Trauma (EFAST). J Trauma. 2004 Aug;57(2):288–95. doi: 10.1097/01.ta.0000133565.88871.e4. PMID: 15345974. ↵

